Testicular Cancer
What is Testicular Cancer?
Cancer is a disease that affects the cells that make up the tissues and organs in the body. Cells normally grow and divide in a controlled way, but sometimes, this process gets out of control and the cells continue to divide to form an abnormal growth or lump called a tumour. Tumours can be benign (non-cancerous) or malignant (cancerous).
The testes (testis singular: both commonly known as the testicles) are a pair of oval-shaped glands that are suspended in a pouch of skin called the scrotum; next to the penis on the outside of the body. Testicular cancer is a condition where the cells within the testis grow and divide abnormally and a tumour grows in the testis.
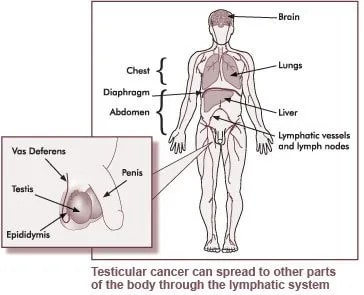
A cancer will usually appear as a painless lump in a testis. If medical attention is sought as soon as a lump, swelling or pain in a testis is noticed, this cancer can remain localised (contained within the testis). However, if left unattended, it typically spreads via the blood or lymphatic system to other major organs such as the lungs.

Gross Appearance of Testis Cancer
Who are at Risk of Testicular Cancer?
Testicular cancer is still one of the rarer forms of cancer with an estimated incidence of approximately 3.8 men in 100,000 men. The risk of being diagnosed with testicular cancer is 1 in 202. In Australia, 850 new cases of testicular cancer were diagnosed in 2016.
Young men are more commonly affected by testicular cancer, with about half of the new diagnoses being made in men under the age of 33 years. Less than one quarter of diagnoses are made in men over 40 years. Testicular cancer is the most common form of cancer amongst Australian men aged 18 – 39 years (excluding non melanoma skin cancer).
There has been a steady increase (2% each year) in the number of men diagnosed with testicular cancer in Australia since 1982 (by more than 50% over the past 30 years). This increase has been greater in other western countries- such as England (3.4% each year) and USA (4.3% each year). The reason for this increase is not yet fully known.
Risk factors for Testicular Cancer
- Undescended testis
- Infertility – is associated with ITGCN (Intratubular germ cell neoplasia). It is not cancer but has approximately 50% risk of transforming into testis cancer within five years. About 5–10% of men diagnosed with testicular cancer have ITGCN.
- Previous testis cancer
- Family History (only accounting for 2% of all testicular cancer)
Despite the increase in the number of new cases, the outlook for men diagnosed with testicular cancer has improved dramatically since the 1970’s when chemotherapy was introduced to treat the disease. The five year survival rate for testicular cancer is 98%. In 2018, there were 34 deaths from testicular cancer.
Types of Testicular tumour
There are two types of Testicular Tumour. The majority will be malignant. These are:
Benign Tumours
A benign tumour is not cancerous as the abnormal cells do not normally invade other tissues or spread to other parts of the body. Benign tumours may cause problems to nearby healthy organs by pressing on them and affecting their normal function if they continue to grow.
Malignant Tumours
A malignant tumour is cancerous as cells continue to grow in an uncontrolled way and can invade nearby tissues and spread to other parts of the body through the bloodstream or lymphatic system. If cells reach a new site they may continue to divide and form a secondary tumour (sometimes called a metastasis), if left untreated.
Stages of Testicular Cancer
The Testis Cancer can be graded based on its aggressiveness and spread.
Staging classification for testicular cancer has become very sophisticated but we have simplified it as follows.
TNM staging system
This is the most commonly used staging system. For testicular cancer, an S is added to the TNM system. Various tests and scans are used to determine this.
- Tumour (T): How large is the testis tumour? Where is it located?
- Node (N): Has the tumour spread to the lymph nodes in the back of the abdomen (retroperitoneum)?
- Metastasis (M): Has the cancer spread to other parts of the body? If so, where and how much?
- Tumour markers (S): Are the serum tumour markers (AFP, beta-hCG, and LDH) elevated? If so, how high are they?
The stage of the cancer will then be assigned by combining the above T, N, M and S classifications.
- Stage 1 – Confined to the testis or confined to the testis with lymphovascular invasion (lymphatic, bloodstream).
- Stage 2 – cancer has shown signs of spread to the lymph nodes in the tummy area (more accurately in the retroperitoneum).
- Stage 3 – cancer has spread to the distant lymph nodes and any organ such as lungs, liver, brain.
Treatment for Testicular Cancer
All testicular cancers can be treated and if discovered early, and the right treatment given, over 95% of them can be cured. Early detection of testicular cancer can lessen the toxic side effects of the treatments used.
Some can be more aggressive than the other types and treatment may be different depending on the type of testicular cancer and if it has spread to other parts of the body. However, nearly all can be stopped with the removal of the testis if confined within the testis. If advanced, chemotherapy will be introduced and additional surgery (Retroperitoneal lymph node dissection, RPLND) might be indicated in small cases.
The outlook is positive for those men diagnosed with testicular cancer. Most men go on to live full and active lives.
Treatment for testicular cancer does not normally affect sexuality, masculinity or erectile function.
While men who go through chemotherapy or radiotherapy as part of their treatment can become infertile, sperm banking before starting this treatment can usually give them the option of fathering children should their fertility be affected.