Penile Cancer
What is Penile Cancer?
Penile cancer is a disease in which malignant (cancer) cells form in the tissues of the penis.
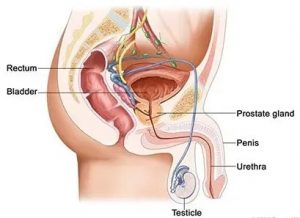
Anatomy of the Penis
The penis is a rod-shaped male reproductive organ that passes sperm and urine from the body. It contains two types of erectile tissue (spongy tissue with blood vessels that fill with blood to make an erection):
- Corpora cavernosa: The two columns of erectile tissue that form most of the penis.
- Corpus spongiosum: The single column of erectile tissue that forms a small portion of the penis. The corpus spongiosum surrounds the urethra (the tube through which urine and sperm pass from the body).
The erectile tissue is wrapped in connective tissue and covered with skin. The glans (head of the penis) is covered with loose skin called the foreskin.
Penile Cancer Symptoms
Symptoms of penile cancer can include the following and other signs:
- Sores,
- Redness,
- Painful urination,
- A lump on the penis.
- Discharge,
- Bleeding
Causes and Risk Factors for Penile Cancer.
Risk factors for penile cancer include the following:
- Being age 60 or older.
- Having phimosis (a condition in which the foreskin of the penis cannot be pulled back over the glans) and chronic inflammation/infection
- Having poor personal hygiene.
- Having many sexual partners.
- Using tobacco products.
- Human papillomavirus (HPV) infection may increase the risk of developing penile cancer. Circumcision may help prevent this infection. A circumcision is an operation in which the doctor removes part or all of the foreskin from the penis. Many boys are circumcised shortly after birth. Men who were not circumcised at birth may have a higher risk of developing penile cancer.
- HIV
- UV-A light (ie. psoriasis treatment)
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer.
Penile Cancer Prognosis
The prognosis (chance of recovery) and treatment options depend on the following:
- The stage and grade as well as subtype of the cancer.
- The location and size of the tumour.
- Whether the cancer has just been diagnosed or has recurred (come back).
Metastatic Penile Cancer
Cancer may spread from where it began to other parts of the body. When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumour) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumour (metastatic tumour) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumour (metastatic tumour) in another part of the body.
The metastatic tumour is the same type of cancer as the primary tumour. For example, if penile cancer spreads to the lung, the cancer cells in the lung are actually penile cancer cells. The disease is metastatic penile cancer, not lung cancer.
Stages and Treatment of Penile Cancer
The Following Stages are Used for Penile Cancer:
Stage 0 (Carcinoma in Situ)
Treatment of stage 0 may be one of the following:
- Topical chemotherapy (5-FU).
- Topical biologic/immuno-modulating therapy (Imiquimod).
- Laser surgery.
- Cryosurgery.
- Mohs microsurgery.
Stage I Penile Cancer
If the cancer is only in the foreskin, wide local excision and circumcision may be the only treatment needed.
Treatment of stage I penile cancer may include the following:
- Surgery (partial or total penectomy with or without removal of lymph nodes in the groin).
- External or internal radiation therapy.
- Mohs microsurgery.
- A clinical trial of laser therapy.
Stage II Penile Cancer
Treatment of stage II penile cancer may include the following:
- Surgery (partial or total penectomy, with or without removal of lymph nodes in the groin).
- External or internal radiation therapy followed by surgery.
- A clinical trial of sentinel lymph node biopsy followed by surgery.
Stage III Penile Cancer
Treatment of stage III penile cancer may include the following:
- Surgery (penectomy and removal of lymph nodes in the groin) with or without radiation therapy.
- Radiation therapy.
- A clinical trial of sentinel lymph node biopsy followed by surgery.
- A clinical trial of radiosensitizers.
- A clinical trial of chemotherapy before or after surgery.
- A clinical trial of new drugs, biologic therapy, or new kinds of surgery.
Stage IV Penile Cancer
Treatment of stage IV penile cancer is usually palliative (to relieve symptoms and improve the quality of life). Treatment may include the following:
- Surgery (wide local excision and removal of lymph nodes in the groin).
- Radiation therapy.
- A clinical trial of chemotherapy before or after surgery.
- A clinical trial of new drugs, biologic therapy, or new kinds of surgery.
Treatment Options for Recurrent Penile Cancer
Treatment of recurrent penile cancer may include the following:
- Surgery (penectomy).
- Radiation therapy.
- A clinical trial of biologic therapy.
- A clinical trial of chemotherapy.
Penile Cancer Diagnosis and Screening
Tests that examine the penis are used to detect and diagnose penile cancer can include the following:
- History and Physical exam: A history of the patient’s health habits and past illnesses and treatments will be taken. An exam of the body will also be performed to check general signs of health, including checking the penis for signs of disease, such as lumps or anything else that seems unusual.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. The tissue sample is removed during one of the following procedures:
- Fine-needle aspiration (FNA) biopsy: The removal of tissue or fluid using a thin needle.
- Incisional biopsy: The removal of part of a lump or a sample of tissue that doesn’t look normal.
- Excisional biopsy: The removal of an entire lump or area of tissue that doesn’t look normal.
The following tests and procedures may be used in the staging process:
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerised tomography, or computerised axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. A substance called gadolinium is injected into a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. The tissue sample is removed during one of the following procedures:
- Sentinel lymph node biopsy: The removal of the sentinel lymph node during surgery. The sentinel lymph node is the first lymph node to receive lymphatic drainage from a tumour. It is the first lymph node the cancer is likely to spread to from the tumour. A radioactive substance and/or blue dye is injected near the tumour. The substance or dye flows through the lymph ducts to the lymph nodes. The first lymph node to receive the substance or dye is removed. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are not found, it may not be necessary to remove more lymph nodes.
- Lymph node dissection: A procedure to remove one or more lymph nodes during surgery. A sample of tissue is checked under a microscope for signs of cancer. This procedure is also called a lymphadenectomy.
Penile Cancer Treatments
There are different types of treatment for patients with penile cancer. Four types of standard treatment are used:
- Surgery
- Radiation therapy
- Chemotherapy
- Topical (Biologic) therapy
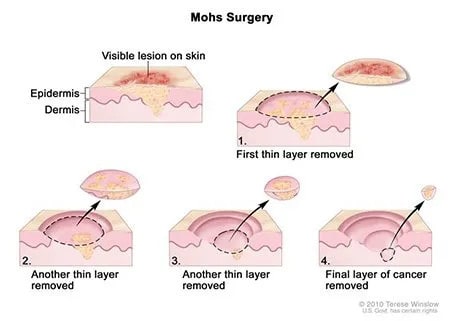
Mohs Microsurgery
A surgical procedure to remove a visible lesion on the skin in several steps.
- First, a thin layer of cancerous tissue is removed.
- Then, a second thin layer of tissue is removed and viewed under a microscope to check for cancer cells.
- More layers are removed one at a time until the tissue viewed under a microscope shows no remaining cancer.
Other Surgical Options
These can include
- Laser surgery: A surgical procedure that uses a laser beam (a narrow beam of intense light) as a knife to make bloodless cuts in tissue or to remove a surface lesion such as a tumour) with Carbon dioxide (CO2) or neodymium:yttrium-aluminium-garnet (Nd:YAG)
- Cryosurgery: A treatment that uses an instrument to freeze and destroy abnormal tissue. This type of treatment is also called cryotherapy.
- Circumcision: Surgery to remove part or all of the foreskin of the penis.
- Wide local excision:Surgery to remove only the cancer and some normal tissue around it.
- Glans resurfacing or Glansectomy
- Partial or Total penectomy (Amputation of the penis): Surgery to remove part or all of the penis. If part of the penis is removed, it is a partial penectomy. If all of the penis is removed, it is a total penectomy.
- Inguinal Lymph Node dissection
- if penile cancer shows adverse pathological risk factors including high stage (T2 or higher), high grade or lymphovascular invasion or palpable inguinal lymph nodes. If the risk of spread to the inguinal lymph nodes are thought to be relatively low, sentinel lymph node biopsy or modified/superficial inguinal lymph node dissection will be performed.
- Sentinel lymph node Biopsy – the sentinel lymph node is the first lymph node to receive lymphatic drainage from a tumour as a sign of spread. A radioactive substance and/or blue dye is injected near the tumour. The substance or dye flows through the lymph ducts to the lymph node. This lymph node is then removed and a pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are not found, it may not be necessary to remove more lymph nodes. It is associated with a lower surgical morbidity or complications but has a false negative rate of 5-10%.
Even if the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that might be left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation Therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing.
There are two types of radiation therapy.
- External radiation therapy uses a machine outside the body to send radiation toward the cancer. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or
- Brachytherapy places a radioactive source directly into or next to the penile cancer. A soft urethral tube, called a Foley catheter, is put through the penis and into the bladder to drain out urine while brachytherapy is done.
The way the radiation therapy is given depends on the type and stage of the cancer being treated.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly onto the skin (topical chemotherapy) or into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
The way the chemotherapy is given depends on the type and stage of the cancer being treated. Topical chemotherapy (5-FU) may be used to treat stage 0 penile cancer
Biologic/Immuno-modulating Therapy
Biologic therapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defences against cancer.
This type of cancer treatment is also called biotherapy or immunotherapy. Topical biologic therapy with Imiquimod may be used to treat stage 0 penile cancer.
Follow-up Testing
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated.
Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
