Prostate Cancer
What is Prostate Cancer?
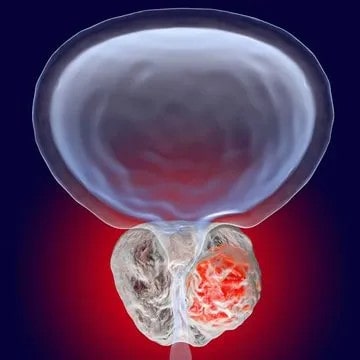
The prostate gland is a secretory gland situated around the bladder neck, and it releases seminal fluid to transport sperm.
Amongst malignancies that affect men, Prostate Cancer is one of the most common types. The overall 5- year survival rate for this cancer is greater than 95%.
While many men die “with” prostate cancer rather than “of” prostate cancer it is important to note that more men die of prostate cancer each year in Australia than women die of breast cancer.
Prostate Cancer
Who Does Prostate Cancer Affect?
Prostate Cancer occurs only in men and is more common in men who are older than 50 years, but it can occur in younger men, especially if there is a strong family history. Therefore, testing for prostate cancer should begin at age 50, or from 40-45 years of age depending on risk factors.
A positive family history on the father’s side of the family (father, paternal uncles, brothers) is the main risk factor and are more likely to result in more advanced cases of the malignancy. Also, a strong family history of breast, ovarian or pancreatic cancer may indicate the presence of a BRCA gene defect which is another risk factor.
The rate of prostate cancer also varies with race, with Asians having the lowest incidence, the Caucasians Hispanics and Blacks having higher incidence rates. However, Asians who have adopted the Western lifestyle have been shown to carry a higher risk of prostate cancer.
How Does Prostate Cancer Occur?
When the cells in the prostate gland become abnormal, this results in the uncontrolled division in the mutated cells, forming a tumour made up of the abnormal cells, which continue to grow and spread to surrounding tissues and potentially to the rest of the body.
Causes of Prostate Cancer?
The causes of Prostate Cancer are still not fully understood. Genetic and racial factors play a role as do dietary factors such as a high-fat diet and obesity.
Symptoms of Prostate Cancer
The symptoms don’t appear in earlier stages of the disease. Therefore, men should not rely on symptoms as a guide as to whether there is anything wrong. Only a PSA test and a prostate examination can indicate whether cancer is present.
As the malignancy progresses, it can cause the following symptoms:
- Difficulty in urination, the need to push harder
- A weaker stream of urine
- Pelvic discomfort
- Blood observed in ejaculation (semen)
- Erectile Dysfunction
- Infertility
- Fatigue,
- Weight loss,
- Bone Pain
Types of Prostate Cancer
Prostate cancer occurs when a tumour develops in the prostate gland. A core distinction with Prostate Cancer is whether the Cancer:
- is localised only in the Prostate, or
- if it has spread outside the prostate gland to the lymph nodes, bones, or other areas. This is called metastatic prostate cancer.
The most common type of prostate malignancy is adenocarcinoma, either acinar or ductal in nature (almost 98% of all cases).
Other rare types include neuroendocrine (ie small call) cancers, sarcomas and others (roughly 1% of all cases).
Gleason Score for Prostate Cancer
Historically, a scale called Gleason score is used for this which gives a score out of 10.
The Prostate Cancer can be graded based on its aggressiveness and spread.
Oddly, the lowest possible number is a score of 6 which means the cancer is non-aggressive. A score of 7 indicates intermediate cancer, and scores of 8-10 mean it’s very aggressive.
The Gleason score is now being replaced with a simpler system called the ISUP (International Society of Uropathologists) classification. This system is based on the Gleason score as follows:
- ISUP 1 – Gleason Score 3+3 = 6
- ISUP 2 – Gleason 3+4 = 7
- ISUP 3 – Gleason 4+3 = 7
- ISUP 4 – Gleason Score 8
- ISUP 5 – Gleason Score 9,10
Nowadays, ISUP is preferred due to it simplicity and less anxiety to patients.
TNM Staging of Prostate Cancer
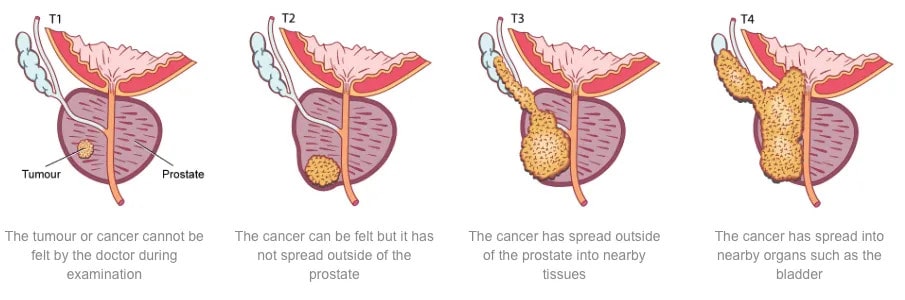
T staging for Prostate cancer
TNM staging essentially describes how far cancer has spread within and/or beyond the prostate capsule. In cases where there is no distant secondaries and where curative treatment is being considered, the T stage is particularly important:
- T1: Tumour is confined within the prostate and the prostate feels normal. It is usually diagnosed on the basis of a raised PSA.
- T2: Tumour is confined to the prostate but the prostate feels irregular to examination
- T3: Tumour has spread just beyond the shell of the prostate into nearby tissue and/or the seminal vesicles at the back of the prostate gland.
- T4: Tumour has spread into adjacent organs such as the bladder, rectum, or pelvic side wall.
Prostate cancer can also spread to lymph nodes (N stage) and to other parts of the body such as to bone and other organs as metastases (M stage).
It is important to note that prostate cancer does not typically produce symptoms until it is advanced. This is why it is important for men to get PSA tests as this is the main way that prostate cancer will be diagnosed before it has spread.
How is Prostate Cancer Diagnosed?
Prostate cancer foundation of Australia (PCFA) and Cancer Council Australia recommend regular PSA screening of healthy men over the age of 50. Earlier PSA screening at the age of 45 is recommended if risk of prostate cancer is increased (ie family history), as early prognosis is crucial for a more positive outcome. Some men present with urinary symptoms that could be related to prostate cancer. However, these symptoms are much more likely due to enlarged prostate (BPH) unless prostate cancer is at an advanced stage.
Screening involves a
- Prostate Specific Antigen Test +/- Digital Rectal Examination
If these tests yield abnormal results, to confirm malignancy and its stage Dr Kim will consider any of the tests listed below:
- Multiparametric prostate MRI
- Prostate Biopsy
- Cystoscopy
- Urinary Flow or Urodynamic Testing
- Other Imaging Tests
Prostate-Specific Antigen – PSA Test
Prostate Specific Antigen is a substance produced almost exclusively in the prostate and plays a role in fertility.
The vast majority is actually released into the ejaculate but tiny amounts are released into the bloodstream and can be detected by a simple blood test. Abnormally high levels of PSA can be an indication of disease of the prostate.
Common reasons for a high PSA level in the bloodstream may include:
- Prostate cancer,
- Large prostates, and
- Age-related inflammation of the prostate
- Infection of the prostate
- Ejaculation, or cycling
Obviously, the first concern is to exclude prostate cancer. Urologist review is advised to exclude this.
Digital Rectal Examination (DRE)
The bladder is the organ that stores urine and the urethra is the tube that drains urine out through the penis. The prostate lies immediately beneath the bladder and completely surrounds the urethra and lies immediately in front of the rectum (back passage).
Dr Kim would normally perform a Digital Rectal Examination (examination via the back passage) of the prostate, an otherwise inaccessible internal organ.
During a Digital Rectal Examination, Dr Kim
- gently inserts a gloved finger into the rectum to feel the condition of the prostate that lies close to the rectal wall. If he feels something suspicious such as a lump or bump, further tests will be carried out.
- Age-related enlargement is not a particular concern but if the gland feels abnormally firm or hard, it may sometimes be an indication of abnormal growth in the prostate gland.
Dr Kim will discuss the test results with you. If anything suspicious is detected such as a lump or irregularity during the exam, further tests will be required.
After the test, you may continue your normal activities.
Prostate Biopsy
This test is commonly performed because either a blood test called PSA is abnormally high or the Digital Rectal Examination (DRE) of the prostate is abnormal. More commonly nowadays biopsy is performed after MRI of the prostate shows suspicion of prostate cancer.
There are mainly two approaches.
Transrectal biopsy
This was the most commonly performed technique. The biopsy needle is passed through the rectum into the prostate. It is quicker and does not need a general anaesthetic. However, due to the risk of serious infective complications Dr Kim does not advocate for this.
Transperineal biopsy
This new technique involves passing the biopsy needle through the perineum which is the area between the scrotum and the anus. This approach is associated with less infection and allows easier sampling in the anterior part of the gland. In addition, more cores can be taken compared to the transrectal biopsy which means that the results can potentially be more accurate. However, it often involves a general anaesthetic, takes longer and may be associated with more short-term urinary flow problems.
Dr Kim performs transperineal biopsy in many different ways (including MRI fusion technology which would help to target the area of concern) to facilitate diagnostic accuracy.
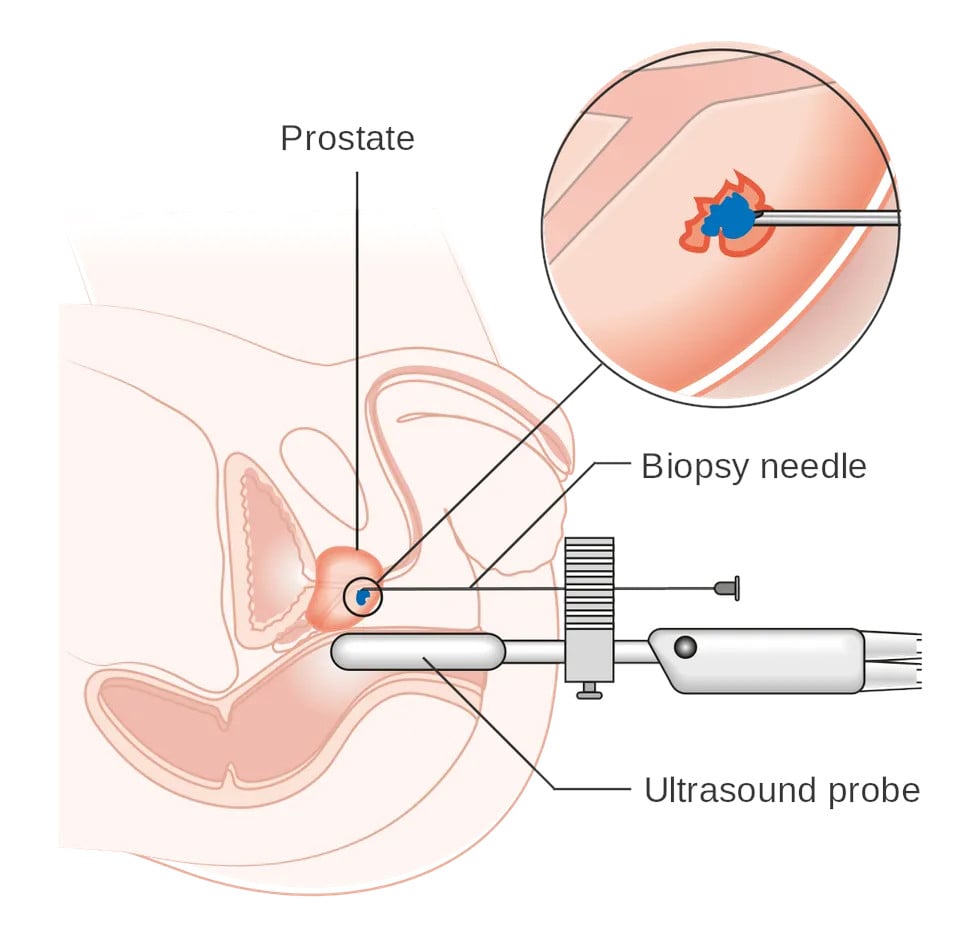
Transperineal Biopsy of Prostate
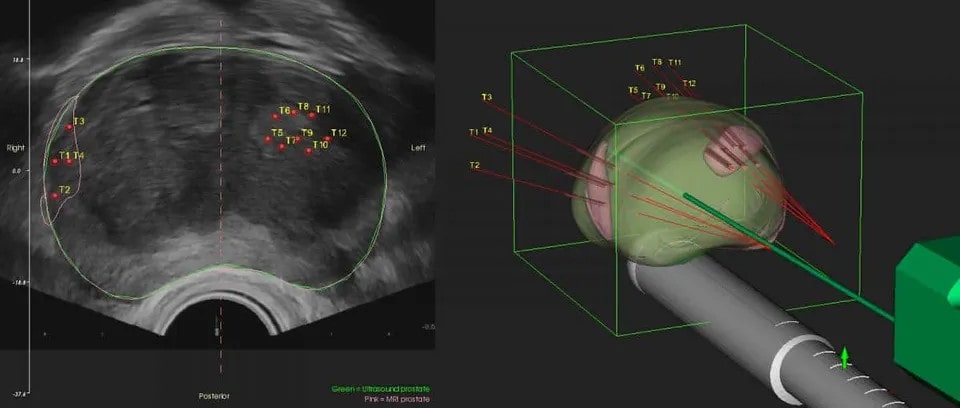
MRI Fusion Prostate Biopsy
Cystoscopy
Cystoscopy enables a urologist to directly view the inside of the urinary bladder and urethra in great detail using a “cystoscope” (the instrument used). There are two types of cystoscopes
Rigid Cystoscope
This is a solid straight telescope and is used with a high-intensity light source. A separate channel allows other instruments to be attached.
Flexible Cystoscope
It is a fibre optic instrument that can bend easily and has a manoeuvrable tip that makes it easy to pass along the curves of the urethra.
This procedure may be carried out under general anaesthesia, although it is normally carried out under local anaesthetic on an outpatient basis.
Cystoscopy may be indicated for the following conditions
- Urinary blockage symptoms due to prostate enlargement, stricture, or narrowing of the urinary tract
- Frequent urinary tract infections
- Blood in your urine (haematuria)
- Loss of bladder control (incontinence) or overactive bladder
- Unusual cells found in a urine sample
- Need for a bladder catheter
- Painful urination, chronic pelvic pain, or interstitial cystitis
- Stone in the urinary tract
- Unusual growth, polyp, tumour, or cancer
Urinary Flow Test
A Urinary Flow Test also known as Urinalysis is a test of your urine.
A urinalysis is used to detect and manage a wide range of disorders, such as:
- Urinary tract infections,
- Prostatitis
- Kidney disease and
- Diabetes.
A urinalysis involves checking:
- appearance,
- concentration and
- the content of urine.
Urinalysis is used to determine the presence of leukocytes (white blood cells) in the urine. Leukocytes help the body to fight infection; a high number indicates a bacterial infection. A urine culture is used to analyse bacteria.
Radiology
Ultrasound
Ultrasound of the prostate uses sound waves to produce pictures of a man’s prostate gland and to help diagnose symptoms such as difficulty urinating or an elevated blood test result.
Prostate Ultrasound can also be used to
- investigate a nodule found during a rectal exam, and provides a visual guide at the time of prostate biopsy
- detect abnormalities in some cases, and
- determine whether the gland is enlarged.
Magnetic Resonance Imaging – Prostate MRI
Magnetic Resonance Imaging (MRI) is a non-invasive imaging technique. This test is similar to a CT scan but uses magnetism instead of X-rays to build up fine cross-sectional pictures of your body. Multiparametric prostate MRI (mpMRI) is an excellent diagnostic adjunct to the evaluation of prostate cancer.
The likelihood of clinically significant prostate cancer is provided using a Prostate Imaging Reporting and Data System (PIRADS) score.
After the above diagnostic investigations
– If clinically significant prostate cancer is diagnosed Dr Kim will arrange a staging scan to ensure there is no evidence of metastasis (spread outside the prostate gland).
Conventionally CT and bone scans are performed.
More recently, a PSMA PET scan have been shown to be more accurate in diagnosing any area of metastasis (spread) than CT and bone scan. Dr Kim will go through the pros and cons of each and arrange appropriate scan.
CT Scan
A CT Scan is an X-ray tube that rotates in a circle around the patient and takes a series of pictures as it rotates. The multiple X-ray pictures are reconstructed by a computer in axial slice images at different levels. Each level can be examined separately.
A CT scan may show if cancer has spread beyond the Prostate to other parts of the body such as the lymph nodes.
The scan takes from 10-30 minutes. You may be given a drink or injection of a dye, which allows particular areas to be seen more clearly. For a few minutes, this may make you feel hot all over. If you are allergic to iodine or have asthma you could have a more serious reaction to the injection, so it is important to let your doctor know beforehand.
You will probably be able to go home as soon as the scan is over.
Nuclear Scans
Bone Scans
This is used to see if the disease or cancer has metastasised and has affected your bones.
A small amount of radioactive material is injected into your arm, abnormal bone absorbs more of the radioactive substance than normal bone and shows up on the scan as highlighted areas (known as ‘hot spots’).
Your arm will then be scanned an hour later to view the activity of the bone and ascertain whether cancer has spread. The level of radioactivity that is used is very small and does not cause any harm.
This scan can also detect other conditions affecting the bones such as arthritis, so further imaging studies such as CT/MRI/PSMA scan of any suspicious area may be necessary for increased accuracy.
Gallium-68 PSMA PET Scans
A small amount of radioactive material is injected into your arm. The radioactive marker then binds to Prostate Cancer Cells. It is combined with Positron Emission Tomography (PET) and CT Scanning technology.
You will then be scanned an hour later to help identify areas where Prostate cancer may have spread to.
Patients only need to present well hydrated and are not required to fast prior to the scan. They are given an injection approximately 45 minutes before the scan which then takes around 30 minutes.
Patients are generally in the radiology department for around 2½ hours in total.
This is a fairly new scan but its accuracy has been demonstrated to be superior to conventional CT and bone scan. Nonetheless, it is not yet covered by Medicare so patients should check the cost of the procedure with the radiology practice.
How is Prostate Cancer Treated?
The treatment of Prostate Cancer varies on a case to case basis. It depends on the
- patient’s age
- general health of the patient,
- cancer’s progression/stage,
- what the overall benefit would be if treatment is provided, and
- consideration of potential side effect profile
The treatment options range widely including
- Active Surveillance
- Robotic Radical Prostatectomy
- Retzius Sparing Radical Prostatectomy
- Radiation Therapy
- NanoKnife Focal Therapy
- Hormone Therapy
- Chemotherapy
- Diet for Prostate Cancer
Patient is also recommended therapy as well as group support for distress and depression that might result from this cancer diagnosis and treatment.
What If Prostate Cancer Is Untreated
If left untreated, the results would vary from case to case.
In some cases, the Prostate Cancer remains confined to the prostate and no other symptoms other than those mentioned earlier are seen. However, in other cases, it may lead to kidney failure or spread to lymph nodes and bones, resulting in further complications and making successful therapy more difficult. Also while the risk of death from prostate cancer over 10-15 years may be low, there can still be considerable pain and suffering requiring intensive treatments in cases where it has spread.
Furthermore, the objective of treatment is to cure the man of his prostate cancer so that he can live his normal full life expectancy.
